It has long been recognized that HIV invades the central nervous system (CNS) at an early stage of infection and drug abuse and alcohol may represent significant cofactors in the progression of HIV-induced neurological disease in minorities. While infection of the nervous system may occur early, because of advances in the treatment, neurologic diseases are a later manifestation of HIV infection and tend to progress in parallel with the degree of immunosuppression. HIV patients who abuse alcohol and/or drugs have compromised immunity as well as nervous system dilemmas. These abnormalities intersect to lead to a constellation of symptoms known as NeuroAIDS.
 The term “NeuroAIDS” includes a myriad of novel neurologic disorders which are a primary consequence of damage to the central and peripheral nervous system by HIV. The medical conditions include sensory neuropathy, myelopathy, HIV dementia, and cognitive/motor disorder. These medical syndromes affect approximately 30 to 40% of adults and children with AIDS, and despite the recent advances in antiretroviral therapy treatment, the prevalence of HIV-associated neurological syndromes is increasing, in part, due to the prolonged life span of individuals who are surviving well on highly active antiretroviral treatments (HAART). However, HAART has chronic and cumulative toxic effects on the already aging brain, which collectively suggest that the burden of CNS complications will increase profoundly over the forthcoming years. Zidovudine (AZT), although effective in treating HIV/NeuroAIDS related neurologic disorders, is limited by its toxicity and the development of viral resistance, particularly in minorities. It has been shown that some HIV drugs are metabolized differently in African-Americans, and drugs such as methadone can inhibit the metabolism of AZT.
The term “NeuroAIDS” includes a myriad of novel neurologic disorders which are a primary consequence of damage to the central and peripheral nervous system by HIV. The medical conditions include sensory neuropathy, myelopathy, HIV dementia, and cognitive/motor disorder. These medical syndromes affect approximately 30 to 40% of adults and children with AIDS, and despite the recent advances in antiretroviral therapy treatment, the prevalence of HIV-associated neurological syndromes is increasing, in part, due to the prolonged life span of individuals who are surviving well on highly active antiretroviral treatments (HAART). However, HAART has chronic and cumulative toxic effects on the already aging brain, which collectively suggest that the burden of CNS complications will increase profoundly over the forthcoming years. Zidovudine (AZT), although effective in treating HIV/NeuroAIDS related neurologic disorders, is limited by its toxicity and the development of viral resistance, particularly in minorities. It has been shown that some HIV drugs are metabolized differently in African-Americans, and drugs such as methadone can inhibit the metabolism of AZT.
“It is estimated that 650,000 to 900,000 Americans” are infected with HIV, 15%-30% of whom will develop some type of neurological disorder, such as neuroAIDS, over the course of their illness. NeuroAIDS affects minorities disproportionately, particularly minorities who are abusers of drugs and alcohol. Racial and ethnic minority populations in the United States, primarily African Americans and Hispanics, constitute 58 percent of the more than 928,188 cases of AIDS reported to the Centers for Disease Control and Prevention (CDC) since the epidemic began in 1980.
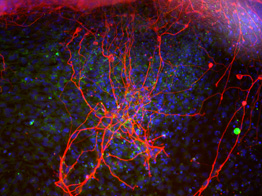
Although the serendipitous means of drug discovery have lead to current therapeutics, there is a need for novel advance modeling system for in vitro experimentation, particularly to study drug design and resistance in minorities who have HIV/NeuroAIDS. Kopnisky et al. states that “Better systems could potentially reduce the amount of time a compound spends in the preclinical development phase and more effectively predict a compounds potential for success in the clinic”. Cellular models are required for drug target discovery, compound screening, functional assays, toxicology, and safety studies, however, traditional cellular models can be poor predictors of functional clinical relevance, in relation to HIV/NeuroAIDS. Jeevan Biosciences is dedicated to the development of human cellular models that represent the genetic diversity seen in the current US population of patients with NeuroAIDS. These cells will be used for drug testing and treatment development.
